Is Bleeding or Spotting During Ovulation Normal?
Whether you’re trying to conceive, trying not to conceive, or in the throes of menopause, bleeding outside of your normal monthly cycle can be alarming. It’s common to worry about irregular bleeding, especially when it is accompanied by other symptoms, or you have experienced health problems in the past. Tidewater Physicians for Women specializes in women’s reproductive health and can help you get to the bottom of it through expert, compassionate care.
What is Ovulation?
Most women have two ovaries, which contain all the eggs they will ever produce by the time they are born. During ovulation, an egg is released from an ovary and travels down a fallopian tube, where it has the opportunity to become fertilized in the right conditions. In some cases, two or more eggs are released (thus explaining fraternal twins, the result of the fertilization and implantation of two separate eggs during the same cycle).
The time of ovulation depends on the length of your cycle. Most women experience ovulation about once a month, and it typically occurs mid-cycle or in the middle of your menstrual cycle. For example, in a 28-day cycle, ovulation occurs about 14 days after the first day of your last period and about 14 days before the first day of your next period.
Many women know when they ovulate based on the signs and symptoms they experience during this phase in their cycle. Common signs of ovulation include an increase in basal body temperature, a surge in luteinizing hormone (LH) levels, cervical mucus that looks like egg whites and is more watery, a change in the position of the cervix, and a positive ovulation test (administered by your doctor or bought over the counter).
Additional symptoms of ovulation include breast tenderness, ovulation pain (mittelschmerz), bloating, and increased sexual desire. These signs and symptoms are so predictable for some women that they depend on them to predict ovulation and prevent conception by using a barrier method of birth control or abstinence during their fertility window.
What are the Causes of Bleeding During Ovulation?
Around 5% of all women who menstruate will notice minor bleeding or spotting during ovulation, which can be explained by hormonal changes. Luteinizing hormone (LH) levels surge 24-36 hours before ovulation. The estrogen levels in your body will rise steadily as your body prepares for ovulation and then suddenly drop once the egg has been released. After ovulation, progesterone levels begin to rise. This hormonal change — as you move from increased estrogen levels to increased progesterone levels — often causes some spotting or light bleeding that is much lighter than typical menstrual bleeding.
Does Bleeding During Ovulation Mean You’re Pregnant?

Bleeding mid-cycle or during ovulation is not an indication of pregnancy. However, it might be an indication that you are in your fertile window, so those who regularly bleed when they release an egg will often either try to conceive or avoid conception, depending on their goals. It can also signify that something more sinister is occurring, especially if accompanied by signs and symptoms of infection like pain, odor, or abnormal discharge.
How Long Does Ovulation Bleeding Last?
While your menstrual period is likely heavier, darker in color, and longer-lasting, ovulation bleeding is much lighter and should only last for a day or two. You can tell the difference between ovulation bleeding and cycle bleeding because ovulation bleeding will be lighter, mid-cycle (about 14 days after the first day of your last period in a 28-day cycle), and possibly mixed with cervical fluid or cervical mucus.
How Much Bleeding Is Normal During Ovulation?
During ovulation, you shouldn’t notice a regular flow of blood. Ovulation spotting is usually light spotting at most: one or two drops at a time. Ovulation bleeding shouldn’t warrant tampon use.
What the Color of Your Discharge During Ovulation Means
The color of your discharge during ovulation could signal various conditions. Here is what each color means.
- Clear to light yellow: A clear to light yellow coloring typically signifies healthy lubrication with not much to worry about. The only problem comes when the color is accompanied by a cottage cheese-like consistency and a strong odor. That could signify an infection.
- Brown: A brown discharge is typically one of the variations of normal spotting, but the timing could indicate another condition. If you see brown spotting before you expect your period, you could be pregnant. If it occurs after you have gone through menopause, it could indicate endometrial cancer in some circumstances.
- Pink: Pink usually indicates a small amount of mid-cycle bleeding, but that can be normal when spotting before a period. If you are in early pregnancy, however, it could be a sign of implantation bleeding. Spotting after ovulation can also be pink, as can discharge after intercourse if there are small tears or irritation in the vagina.
- Green: Darker yellow or green discharge may indicate an infection that’s typically sexually transmitted in nature. If the hue is lighter in color, however, it could simply result from certain dietary supplements.
- Gray: Any shade of gray is typically a sign of bacterial vaginosis, which is a fairly common bacterial infection. It can be treated with antibiotics, but you’ll want to see a doctor as soon as possible.
Does Cramping During Ovulation Mean Pregnancy?
No, ovulation cramping and implantation cramping are distinct, though they may feel similar. Cramping doesn’t necessarily mean that you are pregnant. The only way to know for sure is to take a pregnancy test no sooner than 12 days past ovulation or when you expect your next period to start.
Why Am I Bleeding After Sex During Ovulation?
Bleeding after sex during ovulation can be caused by a variety of factors. One potential cause is friction from sex due to tears in the vagina. This is typically not a big deal, though it could indicate a hormonal imbalance or vaginal dryness if it occurs repeatedly. It could also be a symptom of cervical ectropion, which is a condition in which cells that are supposed to be inside the cervix grow outside of the cervix. This is relatively common and usually harmless, but it can lead to light vaginal bleeding.
Some potentially concerning conditions that could cause bleeding include cervical polyps, endometriosis, and STIs like chlamydia or gonorrhea. It is always best to see your OBGYN to rule out any serious problems.
Why Am I Bleeding Heavily During Ovulation?

Ovulation should be accompanied by light bleeding in the vast majority of cases of mid-cycle spotting. Heavy vaginal bleeding or abnormal uterine bleeding could indicate other problems such as the following:
- Uterine fibroids
- Uterine or cervical polyps
- Hyperthyroidism
- Hypothyroidism
- Polycystic Ovary Syndrome
- STIs
- Cervical cancer
- Ovarian cancer
If you experience heavy bleeding during ovulation, you should see your OBGYN as soon as possible.
When Should I Worry About Ovulation Bleeding?
Normal menstrual bleeding occurs at regular intervals (usually starting every four weeks or so, although every person is different) and lasts between five and seven days. Some women also experience light spotting during ovulation, about two weeks after the first day of their last period or in the middle of their cycle for women who have a cycle that is longer or shorter than 28 days.
Sometimes, irregular bleeding is an indication of an underlying health condition and not just cycle spotting. Some of the most common causes of irregular bleeding outside of ovulation and implantation include fibroids, endometriosis, polycystic ovary syndrome (PCOS), polyps, menopause or perimenopause, pregnancy, and sexually transmitted infections (STIs).
It’s important to see your healthcare provider if:
- You typically experience regular periods and have recently noticed that your menstrual bleeding patterns have changed
- You notice bleeding that doesn’t occur during your menstrual cycle or spotting that doesn’t occur around the middle of your cycle (around 14 days after the first day of your last period)
- Bleeding at any time during your cycle is accompanied by the signs and symptoms of an infection or severe pelvic pain
- You experience ovulation bleeding while taking hormonal birth control (or any form of birth control)
Your physician will ask questions to better understand your history, symptoms, and risk factors; conduct a physical examination; and order additional labs or diagnostic imaging tests if necessary.
How Can I Prevent Ovulation Bleeding?
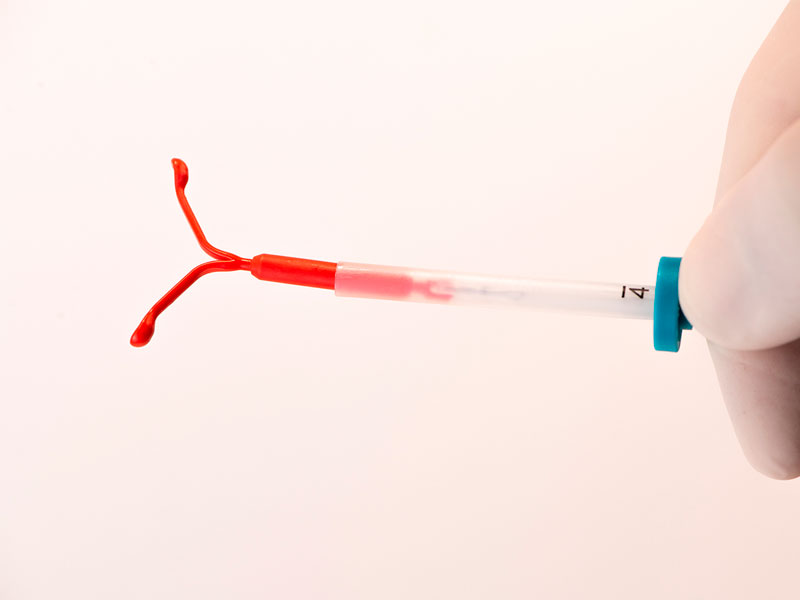
Most women don’t experience ovulation bleeding. Those who do can prevent bleeding by preventing ovulation through the use of hormonal contraceptives, which control hormone levels and stop the release of an egg. Women who are trying to conceive should not take steps to prevent ovulation or any associated spotting.
Tidewater Physicians for Women can help you understand all aspects of menstruating through compassionate women’s health services. Whether you’re ready to start a family, trying to better understand your cycle, or looking for relief from the symptoms of menopause, our team is here to help.
Services available at Tidewater Physicians for Women include:
- Women’s health services, including vaccinations, health screenings, cancer screenings, sex education, menopause treatment, preconception counseling, nutrition screening, and weight control information
- Gynecology services, including birth control, adolescent gynecology, annual preventative care, diagnosis and treatment of gynecological infections and disorders, surgery, and treatment for menopause
- Obstetrics services, including comprehensive care before, during, and after pregnancy including ultrasound examinations and fertility services
- Menopause, family planning, ultrasound, robotic surgery, and more
Even women who do not have concerns about their reproductive health need regular preventative care. Call our office today at 757-461-3890 to schedule an appointment in the Norfolk and Virginia Beach areas.